Sleep plays an important role in physical health and is essential for concentration and productivity. Yet, one-third of adults complain of insomnia. In this post, I explain what insomnia is, what causes it, and how to treat it. I also introduce a 6-week program based on Professor Gregg D. Jacobs’ book “Say Goodnight to insomnia” that I have just started in order to improve my own insomnia.
Several years ago, a friend told me about a superhero comic book. What was special about that comic book was that the characters had useless superpowers. For example, one of these superheroes could become invisible but only when no one was looking at him. Another superhero had the power to predict the future, but only three seconds before it happened, so he never had time to prevent the disasters he knew about before anyone else. The third one knew how events could have gone better… after they had already happened. Well, dear reader, I am about to make a shocking revelation: I’m one of those superheroes.
My superpower is to be able to go into the deepest, most restful sleep in seconds, but only when I don’t need it. This happens maybe once a year, when I’m on vacation, completely relaxed, with nothing important to do. The rest of the time I spend my nights lying in bed, my eyes wide open, and my mind as calm as the opening scene of a James Bond movie.
I suspect that my insomnia is genetic. My parents are also bad sleepers and, since I was a baby, I’ve always had trouble sleeping. Over the years, I’ve read about insomnia and tried to implement some advice, but I’ve never really tackled this problem. I am happy to say that this is about to change.
What is insomnia?
The clinical diagnosis of insomnia is not based on the amount of time spent lying in bed or the amount of sleep. If you sleep five hours a night but feel well and alert during the day, then you do not have insomnia. You’re just a person who doesn’t need a lot of sleep. However, if after a night of disturbed sleep, you feel irritable, tired, or less productive, then you may be diagnosed as an insomniac. It is normal to suffer from insomnia in response to certain life events, such as a break-up, death, health problems, or work-related stressors. However, when insomnia lasts more than a month, it is considered chronic.
There are two different types of insomnia. Staying awake in bed for at least half an hour before falling asleep is called sleep-onset insomnia, while waking up at night and staying in bed for at least half an hour is called sleep-maintenance insomnia.
What are the causes of insomnia?
Psychological causes
Stress and daytime anxiety are one of the main causes of insomnia. Going to bed with a racing mind prevents sleep from occurring. Before falling asleep, many people still ruminate about what happened during the day or worry about what will happen in the future. Their brain awakening system does not give way to their sleep system and they cannot fall asleep.
Another important reason why people cannot sleep is related to their attitude towards sleep. This is the paradox of the useless superhero: the more you try to force sleep, the less you can. Sleep occurs when you relax and let go of intentions. But insomniacs usually worry about not getting enough sleep, and that very idea keeps them awake.
Interestingly, we don’t need as much sleep as we often think we do or are told we do. Have you heard that we should get eight hours of sleep a night? I have heard it. And I’m constantly trying to get at least seven hours. Well, research shows that five and a half hours are enough to function during the day. That’s called core sleep. Five and a half hours of core sleep contain 100% of the deep sleep needed to function normally. That is why parents of young children, physicians, surgeons, soldiers, and astronauts, whose sleep is drastically depleted and interrupted, are still able to function at a high level.
Physiological causes
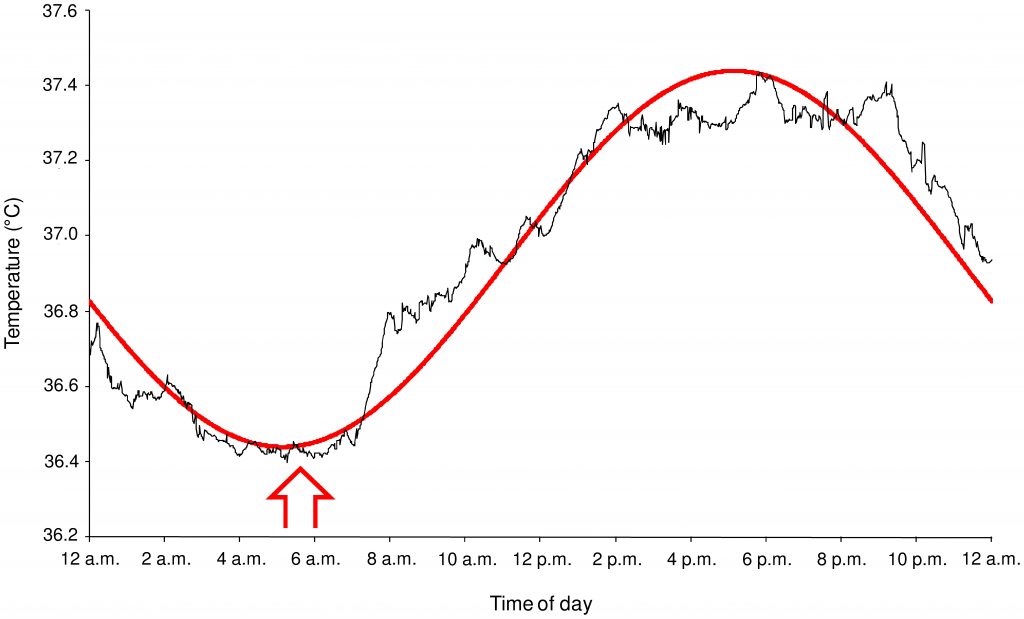
Studies on the physiology of sleep have revealed the importance of body temperature. Body temperature varies throughout the day. It increases in the morning (from about 5 a.m.) until late afternoon (about 6 p.m.) and then decreases during the night. Circadian (i.e. daily) variations in body temperature appear to play an important role in regulating the brain’s wakefulness and sleep systems. It is therefore not surprising that insomniacs exhibit disruptions in their body temperature rhythm. Research on sleep-onset insomniacs shows that their body temperature drops later in the night than that of good sleepers, which may explain why they need more time to fall asleep. Similarly, studies of sleep-maintenance insomniacs show that their temperature does not drop as much during the night, which may affect the depth of their sleep.
Medical conditions
Certain medical conditions and symptoms are known to disrupt sleep, such as:
- medical problems that affect breathing (for example, asthma, bronchitis, allergies, cough, sleep apnea)
- pain (for example, arthritis, headaches, chronic pain)
- bladder problems that lead to frequent urination
- hyperthyroidism
- brain diseases (for example, epilepsy, dementia, and Alzheimer’s disease)
- kidney disorders
- diabetes and hypoglycemia
- menopause, premenstrual syndrome, and pregnancy
- mental health problems (depression, anxiety, post-traumatic stress)
- periodic limb movement, restless legs, bruxism (teeth grinding)
Medication or substance use
Some medications or substances also seem to interfere with sleep. Caffeine and alcohol are, of course, harmful to sleep if taken in large quantities. The same is true for illicit drugs, especially cocaine and amphetamines, but also, in some cases, marijuana, as well as some prescription and over-the-counter drugs.
How to treat insomnia?
The cure for insomnia depends on its causes. Of course, the first thing to consider is whether you have a medical problem or are taking medication that could interfere with your sleep. If you think this may be the case, it is recommended that you consult a doctor.
Many people turn to sleeping pills to help them overcome insomnia. However, in most cases, sleeping pills are a bad idea. Many drugs sold or used as sleeping pills (e.g. antihistamines, painkillers, melatonin) have no scientifically proven effect on insomnia other than the placebo effect. Sleeping pills that have a scientifically proven effect on sleep, such as benzodiazepines and antidepressants, are not necessarily better. They can alter the quality of sleep and cause side effects and dependency. Therefore, regular use of sleeping pills is not considered safe and is not recommended by medical authorities.
The first treatment recommended by experts to treat insomnia is cognitive-behavioral therapy (CBT). CBT provides psychological and behavioral methods to control or eliminate the negative thoughts and actions that keep insomniacs awake. This approach is drug-free, safe, and has been tested in hundreds of scientific studies. The results of these studies show that 70-80% of insomniacs who have completed a CBT program experience lasting benefits from the treatment. Not bad, isn’t it?
The CBT program I decided to try is described in the book “Say good night to insomnia” by Dr. Gregg Jacobs. Jacobs developed and tested his program as he was an assistant professor of psychiatry at Harvard Medical School. The first edition of his book was published in 1998 and since then it has been one of the best-selling books on the subject. Jacob’s method has been scientifically tested and published in peer-reviewed journals. The whole program is described in the book, so it is cheap and requires nothing more than reading the book and following the procedure it describes.
How does the program work?
It is a 6-week program that targets the psychological, behavioral, and environmental causes of insomnia. For each week, the book provides practical exercises and instructions.
- Week 1 consists of changing your thoughts about sleep
- Week 2 aims to establish sleep-enhancing habits.
- Week 3 deals with lifestyle and environmental factors that affect sleep.
- Week 4 offers techniques to promote relaxation.
- Week 5 teaches how to relieve stress
- Week 6 is devoted to developing attitudes and beliefs to reduce stress and improve sleep.
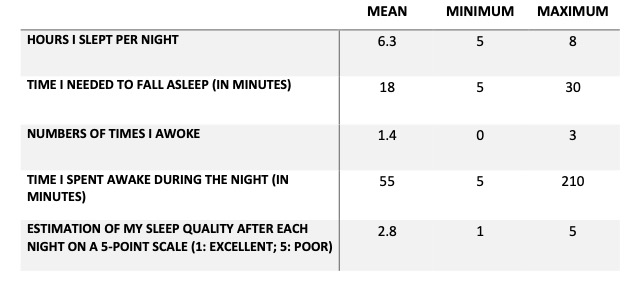
I’m already one week into the program. The first week consists of learning how sleep works (including some of the information described above) and assessing one’s baseline sleep. Below you will find my data for the last 7 days, i.e. before the start of the program. Of course, these data are in no way scientific evidence. But it is still better than a subjective feeling, and why refrain from creating an Excel spreadsheet and running a good old-fashioned ANOVA when it is served on a gold plate.
I’ll let you know how my sleep progresses. Wish me luck… and good night!
Gaya
Cover photo by Guzmán Barquín on Unsplash
Pingback: Deliberate cold exposure for focus : A Brilliant Mind